Fetus in utero, between fifth and sixth months. Image credit: Wikipedia. Regenerative medicine is a new and expanding area that aims to...
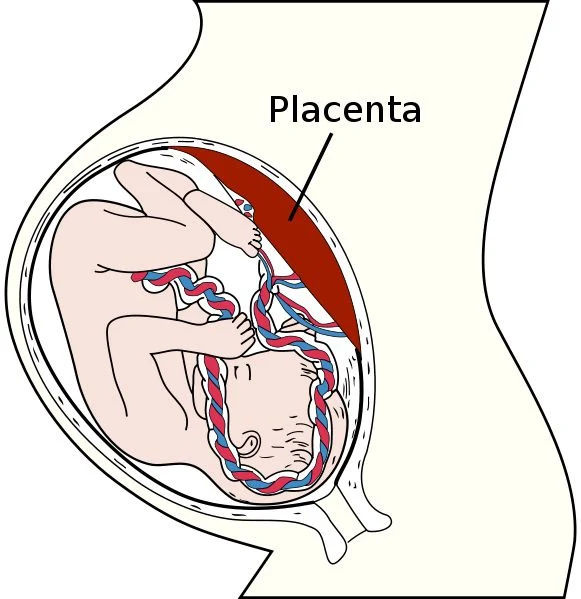 |
| Fetus in utero, between fifth and sixth months. Image credit: Wikipedia. |
Two Japanese scientists, Nobel laureate Shinya Yamanaka and Kazutoshi Takahashi, showed, in 2006, that introduction of four genes in skin cells can reprogram fibroblasts into functional embryonic stem-like cells (also termed "induced pluripotent stem cells" ("iPSCs"). The notion that as little as four genes are sufficient to reset the epigenome of a cell, opened a new avenue where scientists have attempted to convert different adult cells into other somatic cell types. Several subsets of cell types such as blood cells, nerve cells, heart cells and liver cells were converted from different adult cells by employing the direct conversion approach.
This discovery opened an attractive avenue that resolves both the ethical issue and the immune rejection problem of ESCs and the need for donor cells.
The placenta is the least understood human organ, but arguably one of the most important ones. It influences not only the health of a woman and her fetus during pregnancy, but also her lifelong health.
Placental insufficiency occurs when the placenta does not develop properly, or is damaged. Placental dysfunction diseases are associated with low birth weight, premature birth, and birth defects. One such disease is fetal growth restriction (FGR, also termed intrauterine growth restriction [IUGR]), that tends to display mild mental retardation and in severe cases causes fetal death. They also carry increased risk of complications for the mother. To date, tools to model or treat these diseases are limited because all attempts to isolate and propagate the human placenta precursor cells (i.e. trophoblast stem cells, cells that can form the placental cells) in the dish have failed.
Now, researchers from the Hebrew University of Jerusalem, led by Dr. Yosef Buganim of the School of Medicine-IMRIC-Developmental Biology and Cancer Research, have succeeded in converting skin cells into stable and fully functional induced trophoblast stem cells (iTSCs, the stem cells of the placenta that responsible for the formation of most cells in the placenta). These skin-derived TSCs look like native TSCs, and function and contribute to developing placenta.
The success of this study will grant a real chance for women who suffer from placental dysfunction diseases to have healthy babies. It is important to note that these cells do hold any risk since they integrate only into the placenta and not to the embryo himself.



No comments